Other Categories
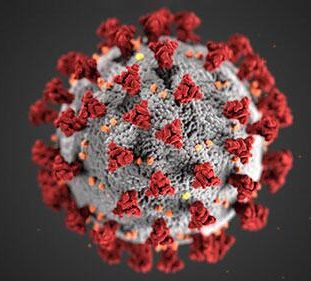
The COVID-19 pandemic has given us a new appreciation for the role of public health. While our public health departments and hospitals continue to manage vaccination and cases resulting from new variants, we also know that those of you battling C. diff infections still need our help. Please know that we are still here for you through our Facebook page, C. diff Support Community and through our Contact Page.
We are also working with members of our Scientific Advisory Council to field and answer questions about C. diff and COVID-19. Please note that this is not medical advice. We are just providing general information to help guide your conversations with your healthcare providers.We will continue to update this blog post with additional questions and answers as we process them.
COVID-19 and C. diff Frequently Asked Questions
Will the mRNA vaccines the prevent COVID-19 infections make me vulnerable to a new or recurrent C. diff infection?
There is no evidence that any vaccine to prevent COVID-19 increase risk for C. diff infection, nor any plausible reason to think that may occur. These vaccines are not antibiotics. In fact, getting severe COVID and requiring hospitalization (and then potentially requiring antibiotics) may increase risk for C. diff so vaccination, by protecting against COVID hospitalization, may indirectly protect against C. diff.
Does having an active C. diff infection make me more vulnerable to coronavirus?
Possibly. Because the same loss of colonization resistance (having a health gut microbiome) that predisposes to C. diff infection may predispose to susceptibility to COVID-19, which does appear to have enteric transmission (can be transmitted by the mouth into the intestines).
Are people who have recovered from C. diff considered “immuno-compromised?”
Not necessarily, unless the patient also has another underlying health issue (related or unrelated to CDI).
I had a fecal microbiota transplant (FMT) for C. diff. Does that make me more vulnerable to COVID-19?
We asked three doctors who perform FMT. They did not believe C. diff survivors who had recovered through FMT were at increased risk for COVID-19. They even suspect that some FMT recipients may have slightly better immunity, but there’s no data at this time.
Can COVID-19 be transmitted through a fecal microbiota transplant (FMT)?
Possibly. On March 23, the FDA issued a Safety Alert regarding the possible transmission of the virus that causes COVID-19 through fecal transplant. Read more on our blog.
Can the drugs being used for COVID-19 reactive C. diff infections?
There are, at present, no drugs that have been definitively shown to be effective against COVID-19 specifically. There are investigational therapies that are being evaluated in clinical trials, including agents that are known to increase risk of CDI. COVID-19 can lead to bacterial infections requiring antibiotics, which can also increase risk of CDI.
Does actively taking vancomycin deplete my immune system?
No. It is unlikely that actively taking vancomycin would significantly reduce the numbers of immune cells or otherwise impair the immune system acutely. Patients taking vancomycin for C. difficile should not discontinue vancomycin because of concern of COVID-19. However, vancomycin may also have risks relating to COVID-19 that have not yet been identified.



Recovered from covid and the next week tested positive for c-diff. Can you get c-diff from covid? Was not hospitalized and have not had antibiotics in a long time.
Same scenario. 3 months of gastric hell since positive Covid test. Starting second course of vancomycin. Never even had a fever.
I also have had cdiff for 3 months and am starting my fourth round of my vancomycin. The other antibiotic is $1000☹️
Dificid works best. Worth $1000 if you can get it for that.
Dificid kicks it.
Take probiotics after. Clean (esp bathroom) with Clorox)
Call the company. They have a program for those who can’t afford
What program?
I was diagnosed with C diff. I did research and found the miracle cure in addition to probiotic and vancomyicin was Oreganol Capsules. Oregano kills bacteria. You need to take the capsules so they reach the intestinal tract. My doctor was willing to try it. I purchased at a respected health store that sells supplements. Dont purchas from places like Walmart, CVS. I have not had problems and am happy to report I am through with c diff. Good luck.
My husband got his second covid vacine. 3 weeks later he is diagnosed with c diffe.
I am on vancomycin and have been on vancomycin since 2019 because of reoccurring cdi. I worry that I can now be immune compromised.. can daily intake of 125×3 a day longterm create immune issues..
I got C Diff for the first time in my life when I had COVID. However, mine was caused by a combo of my weakened immune system plus my dr prescribed amoxicillin and a steroid because he thought I had a sinus infection.
I had an outbreak at my job and got tested. My Dr said that I could just stop taking the meds when I got a positive test result, that I would be fine but I wasn’t.
After 14 days of horrible COVID symptoms, I tested negative and went back to work. They were giving the vaccine and my Dr told me I should get it even though I had just returned to work 2 days prior. He said I would be fine.
I got the vaccine and I was so far from ok. Vaccine made me feel like I had COVID all over again. Plus it exacerbated and prolonged C Diff infection I didn’t even know I had. I fought C Diff from the end of January to mid-July.
I was getting better and felt great UNTIL I was mandated to get 2nd shot recently because I am a healthcare worker. Now I am rushing to the bathroom at least 3X every morning. I have to take my stool sample in to get tested this morning. I am ordering Banatrol as we speak. If I am positive, my GI is ordering DIFICID. My insurance covers 4,000mg a month and my copay is $70. I’ll take it.
If positive, this will be my 3rd recurrence and it means that Flagyl and Vanco did not work.
It seems as if COVID and the vaccine are causing all types of damage in people. When I read the phrase “no evidence has been found” it frustrates me because there is evidence all over C Diff support groups that there is a link between COVID and increased C Diff infections.
We may not have medical degrees but most people know their body and can tell when something has negatively impacted their health.
I hope everyone here recovers from their infection. This is a terrible illness and needs more research and in my opinion, needs more media attention because it is life threatening but not many people have heard of it.
Hi Amanda, I am so sorry for your struggle with C. diff and COVID. However, we stand by there being no evidence of the mRNA vaccines are contributing to C. diff recurrences. We’ve heard from a few people who have had a C. diff recurrence around the time they received their first or second shot. But as far as we can tell, it’s an issue of correlation not causation. In other words, these people were likely to get a recurrence for reasons that have nothing to do with the vaccine, and it’s a coincidence that it happened after they received their shots. This is because there is no evidence that the mRNA vaccines cause disruption of the gut microbiome. We remain open to additional research and updating the information we’re providing.
They need to keep investigating, because there is definitely a correlation. Better yet, they need to come up with a better vaccine safe for those of us who suffer with these intestinal disorders and diseases. No more assumining just ‘because’ there ‘appears’ to be no correlation that an mrna shot can bring on c dif and other related issues. It’s doing something for sure. Thank you for being here for us.
After receiving my second dose of Pfizer, 4 days later, I have also develop C-Diff. Not sick in any way, and not taking any antibiotics prior to getting C-Diff. From what I have been reading from various people, there must be a correlation of the two.
I was 7 weeks out of a FMT and relapsed a week later. When through the protocol and had a 2nd FMT. Was 3mos out and was advised to get the 3rd shot. I’m currently waiting on my results to come back. One time may be a coincidence but 2x….
It also happened to someone else in my C-Diff support group
I think there’s more to this. Just my opinion.
You need to keep researching. I am another patient that got C Diff after my 2nd Pfizer vaccine . I wasn’t on any antibiotics prior to vaccine
I got the vaccine right before I got Cdiff for the first time, I wasn’t sure if I should call CDC back to tell them that I had gotten the shot just prior. The cdiff I got was the one from murky salt water or uncooked seafood. I have not gone in the ocean and I hate seafood.
I got my moderna vaccine and got cdiff. I have never had antibiotics and hybernated for two years.
I have had three recurrences now and this cdiff is deadly
I have been fighting cdiff for 6 months . finally took dificid . Vanco didnt work . Tested negative yesterday but have had a false negative before so will retest in 2 weeks. i am supposed to get covid booster shot in 2 days . Omg afraid to get covid and get cdiff but will vaccine make it come back?? what do i do??
To our knowledge, there is no relationship between the COVID vaccines and C. diff infections.
I too had a booster last October and c.diff diagnosed after three dreadful months. I’m down for another booster today and scared it will aggravate c.diff. Took vancomycin a couple of months ago but still got c.diff. A terrible scourge to live with.
I would not get another covid booster with your history.
I last had CDiff 9 years ago after taking antibiotics. It flared up literally the same day I got the Covid vaccine. I was dealing with it but when I got the second shot 4 weeks later, it got severe. Bloody, lime green stools off and on for weeks. Ridiculous gas constantly blowing up my gut. The blood and pus went away after around 6 weeks. Now, 8 months later still not back to normal. I will not get boosted. There is a correlation period!
Are you being treated for the C. diff? It’s possible that there is a correlation but that doesn’t mean the vaccine is causing C. diff to return. There are so many factors, which are worth investigating.
Same happened with me. got my booster and I thought the GI issues that came with the fever I got from the booster were going to go away in a few days, that didn’t happen, I have been super sick with neurological issues, making going to the bathroom difficult, having to take medications, not antibiotics though because of all the pain the booster caused, that even after 8..12..14 weeks never went away and got worse..then I actually got covid 14 weeks post booster, still no antibiotics taken, or steroids, just cough meds and tylenol, the diareha started bad with the covid..didn’t get better when covid symptoms went away. tested positive for c-diff and both toxin A & B. my GI said they are seeing a lot of GI issues, inflammation in the GI related to covid and people getting C-Diff for first time or a relapse..they cant find a correlation to the vaccine..but can to having covid for sure, antibiotics or not. It’s horrible and doctors need to be aware that Dificid is the now top tier medication to kill it and prevent a replapse, they need to stop prescribing flagyl and vanco as first tier and get these insurance companies on board for paying for dificid faster to stop the spread of C-Diff in the community and the hospital. The fact they made a healthcare worker go to work with actice C-Diff is pretty disturbing. When I have C-Diff and am in hospital I’m quarentined, people gown up to come into my room, and they tell me not to use a public restroom until I am better.
I wish the government would emergency approve the fmt pills ..
In my experience, while a person is being treated with antibiotics, they needs to be taking probiotics (at least twice a day – that’s per an “Infectious Disease Specialist”).
C-DIFF is kind of like “trench warfare” in the First World War – “Bad guys” have taken over some, most or all of the “friendly” territory. The antibiotics are like bombardments – the kill off the “bad guys”, but they also kill off most of the “good guys” in the process. If we don’t send in more “good guys” to hold the territory, the “bad guys” just move back in. The Probiotics are the good guys for the intestines, where C-DIFF dwells. Then the “hold-outs” have to be addressed.
Re-infection is not unusual (though it is discouraging.
Re-infection from one’s personal environment (i.e. – where you live) is not uncommon. The “C-DIFF spores” are viable for possibly a year or more. So, another thing that I did was to disinfect my entire apartment. I used “Professional Grade” disinfectants, to the extent that I could (Clorox ‘Fuzion’ for “hard surfaces”). The “dwell time” (the amount of time that the surface has to remain wetted with the disinfectant – also known as “contact time”) is important The “dwell” time for Clorox Fuzion against C-DIFF is 2 minutes. I used the “Oxy” type cleaners for “soft” surfaces (i.e. – carpet and upholstery).
No subsequent problems, and my infection was “severe” (“Acute”) (the C-DIFF toxins damaged several organs).
Can I take the booster vaccine if Im on vancomycin for cdiff ?
Moderna vaccine, is it safe if I’m on Vancomycin. The day I’m having the Moderna Booster, that morning is my last pill and shot is at 1:00 p.m.
i am in the same situation. I just finished dificid and have appt. for booster in 2 days unsure of what to do. if you get answers please share
If I had Covid and did not take any antibiotics, and have never had C diff, is it possible to get c diff simply from having Covid infection?
I had my first Pfizer dose on a Friday in August, had emergency surgery that Tuesday to have my appendix out. (No issues prior to vaccine. Had stomach pain and heart burn hours after vaccine ). Had to be treated for an abscess from the surgery, then almost had Gallbladder surgery because the extraction rate is super low, then H.pylori, then C diff. And the biggest kicker, I have COVID so the vaccine didn’t even do it’s job (had it 8/27/21-less than 4 months ago). I am tired of people telling me this is all a coincidence because it’s certainly not. And now that I tested positive yesterday, it just proves my body rejected the vaccine. But my employer requires it and of course, doesn’t want to hear anything about my issues
My father is very sick in hospital at minute with C-diff ,got vaccines a couple of weeks before ,there no let up with it ,any advice greatly appreciated hes 88 next month
I am passing block everytime I have a bowel movement. I had C-difff in the past and was told not to take antibiotics any more. I did get the Covid Shot and now I am passing blood again during all bowel movements. Could the Covid shot be causing this?
I am passing blood everytime I have a bowel movement. I had C-difff in the past and was told “not” to take antibiotics any more. I did get the Covid Shot and now I am passing blood again during all bowel movements. Could the Covid shot be causing this?
My daughter developed C. diff after getting a mild case of COVID for which she was prescribed antibiotics. According to her gastroenterologist C. diff can be antibiotic induced and/or an opportunistic infection that flares up when a viral infection stresses the GI lining. It is possible that COVID could result in conditions that make the GI system susceptible to being taken over by C. diff, especially when it is known that the Delta variant can cause diarrhea as a symptom.
I got my moderna vaccine and then got cdiff I have not been on antibiotics in years and was pretty much isolated since the pandemic. Now we are in April 2022 and I have had a third recurrence and I feel like I am dying. It is awful. I feel like the moderna vaccine and all these peoples reports are proving the case. I researched ingredients in vaccines before I got mine and found nothing online back in 2021 what was in each vaccine pretty scary
I’m interested in the same thing. I had a very bad upper respiratory illness for four weeks, followed by diarrhea. Tested positive for c diff. It’s been two months of living hell. I’ve lost 13 pounds and vancomycin is worst antibiotic I’ve had. I had not taken antibiotics in 20 years.
I don’t believe you can get C. diff from COVID. However, if your body is battling a virus and you’re not able to eat well or your overall immunity is suppressed, it may make you more vulnerable. Unfortunately, I’m not aware of any research on it yet. There was a small study done that showed C. diff in COVID patients but they all had taken antibiotics.
I just got over cdiff is it safe to take a covid shot ? And reintroduce antibiotic yo my body which is in a covid shot?
I got the first shot and got cdiff took antibiotics then received the second shot and got cdiff again so beware Goodluck
Dificid works best. Worth $1000 if you can get it for that.
Dificid kicks it.
Take probiotics after. Clean (esp bathroom) with Clorox)
Me too.
I just posted about being in a similar situation. They say there’s no correlation but I’m questioning that.
Good luck.
I have the question as yours. Hope someone can help with this question.
I have the same question as yours. Hope someone can help with this question.
Dificid is the antibiotic that helps me when I have Cdiff
Vancomycin was terrible
Once you took that medication did your c diff come back
I had C-dfff and had the trans plant and got rid of it. I was told by the doctor not to take antibiotics anymore. I got the Covid shot earlier this year and now I am passing blood again but it is not Covid. I am waiting to have a scope done but I know it is not C-difff
So I meant not C-difff
Kirsten cdiff is hell. I am on my third recurrence vancomycin does not work…I got my moderna vaccine and booster and then got cdiff. Pretty scary
I previously had C.diff. I am 78 and have high blood pressure and have been diagnosed with chronic kidney disease. Given the latter two underlying health issues, does C.diff make me more vulnerable to Covid 19?
Hi Jim, I’m not aware of those making your more vulnerable to getting infected by COVID-19. But it does mean that you’re more likely to have a worse outcomes. So stay safe
Can being COVID positive make c diff flare up or return? I have not had c diff symptoms for years prior to this.
Not to my knowledge but it is a new disease so it’s worth checking with your doctor.
Today, is exactly why I am here reading this board. I did not get the Covid shot and thank goodness, my doctor was recommending the shot to all patients except for people like me, so we were actually on the same page. I thought I had the flu this past weekend and 3 days ago, because of some respiratory issues that popped up with this “flu”, I think I have caught Covid. I had diarrhea starting yesterday, but only a few times, inconvenience but not too big a deal. BUT, this morning rushed to the bathroom after I got up and I can honestly say my colon is feeling just like when I had C. diff 3 years ago. And I am not going to post a tome here but I assure you I am not about due for a recurrence anytime soon, as suggested up above by Christian.
If the distinctive odor comes back (and if you have had C.diff you know exactly what I mean), I will most certainly have proof then and can contact doctor for more treatment. Crossing fingers this is NOT the case-more afraid of C.diff than most things after what I went through.
Also, I was reading someone said if they test positive again (3rd time I think?) for C. diff, well, I am not trying to be a know-it-all but research this. Once you have C. diff you will ALWAYS test positive for C. diff. I mean sure, they can waste your money testing it, but if you test 5 years from now, you will still be positive for C.diff. The only thing they can do, is test you for all the others that were originally negative and if they stay negative, it’s safe to assume C.diff. But if your doctor knows, and you know, treatment is the only help at that point.
I had surgery was in the hospital for about a week and in that time i got c diff i just finished taking the antibiotics and ive just tested positive for covid and im worried i have really bad abdominal pain and diarrhea my mouth tastes like metal im scared to go back to the hospital because i dont want to worsen my infection
I had my first COVID shot February 1st.
On February 5th I got diverticulitis, taking antibiotics. Now I may have c-Diff colitis!! Can I still get my second shot when it’s due while I have c-Diff colitis?
I am in the same situation, I got the first shot and got pneumonia and had to take antibiotics and vancomycin and a probiotic, now I am due for the second one tomorrow and I don’t know if I have c-def again or not there is no time to test.
What did you end up doing?
I had c diff over a year ago. I got the 2nd covid shot today. Will the covid shot make my c diff come back? I have been going number 2 alot today but i dk if its bc of the food i eat
Agree. I wish someone could help address this question. I have had reoccurring cdiff but clean for about 4 months now. Got 1st Covid vaccine and now seem to have cdiff symptoms. Didn’t consider that vaccine would cause this issue.
Antibiotics in C19 vaccines? Yikes.
That should be disclosed esp for those who have c diff recurrences
Marilyn You may not have had diverticulitis. I got my covid shot started having pains they told me i had diverticulitis and treated me for that..but all the while I Had cdiff because when they saw the diverticulitis antibiotics did not work they tested me for cdiff I have had it for three times now
25 yrs old. Tested positive for COVID took antibiotics and I now have C. Diff!
I am sorry to hear that. Let us know if we can help. – Christian
I have previously had c diff. I worry about taking any medications and refuse antibiotics. Could the Covid vaccine have any chance of bringing c diff back?
I’m in the same situation, did you got the vaccine? If so how did it go?
Is it safe to take Covid vaccine with an active c diff infection?
Im 25 and had a bout of c. Diff a little over a month ago. I am still having symptoms after one round of antibiotics but they arent bad enough to treat with another round. I have been working hard with my diet and probiotics to make myself heal but now my roommate has covid and im kinda freaked out that i could have it and have c. Diff. Do you guys reccomend florastor or any other probuotics to help me out? I really just want to heal this before/if/when i have covid
Hi Marina, I’m sorry to hear about your battle with C. diff. I imagine that having your roommate be positive for COVID is doubly scary. Unfortunately, we can’t provide specific medical advice. I recommend you speak with doctor treating your C. diff and ask what you might be able to do.
Hi Marina,
I had a bad case back in January of C-Diff. It took me two rounds of vancomycin and changing my diet completely. I cut out all gluten, no coffee, no alcohol & took florastor. I healed. However just got diagnosed with Covid 10/31 had to take antibiotics and feel like it’s coming back. Still fighting covid & praying this doesn’t weaken my immune system even more. Wishing you all the best. Just know diet plays a big role in your c-diff recovery
Hi Claudia,
Did you take the florastor with the antibiotics? Did you take any other probiotics along with the florastor beings it’s only one strand? My Dr told me to take Align following treatment but I’m not so sure about it.
Thanks!
I personally went with Just Saccharomyces Boulardii by the brand Nexabitic when I had c.diff. Along with the Vancomycin. Took 2 a day. I was battling c.dff for nearly 5 months straight. I did a lot of reading up and I seen the boulardii was very good against it. It did seem to help me. Now anytime I get even a thought about it. I’ll take at least one of those to make sure. So far so good. Nearly a year in the clear. Though I’m afraid to take the covid shot after reading some of the stories here.
Did you get the Covid vaccine
It is 2022. I had cdiff in March
What are studies about getting vaccine
Does it cause relapse of cdiff
I am taking dificid for c diff and was given floristor to take at home. I just got out of the hospital. They diagnosed me July 30th with diverticulitis . It only got worse. After 4 visits to the ER then finally a colonoscopy was I diagnosed with C Diff. I was hospitalized and put on vangomiacin that didn’t work. Finally the insurance company approved dificid. They sent me home with 15 doses, which I’m still taking. Hopefully, this takes care of it. I’ve never been so sick!!! My thoughts and prayers are with anyone going through this. ❤????☹
I had C-dff Colitis last
Aug.2020; am I in a higher group to catch Covid 19?
It seems that CDIFF patients are at more risk for worse outcomes with COVID-19. Would it be possible for people with CDIFF to be able to get the vaccine at the same time as immunocompromised individuals. If so, how?
To my knowledge, C. diff patients don’t get any preferential treatment in terms of getting the vaccine earlier.
If I have c diff can I get the covid vaccine
I currently have CDIFF and just started Vancomycin. I was supposed to get my first Covid shot today. VA pharmacist said it was ok, but my GI doc said to wait 2-3 weeks. Anyone else in this boat ?
I am and don’t know what to do I just got the call for shot tomorrow. Don’t know what to do
Yep. Not getting shot around time my body is dealing with C diff.
No way
I have had C Diff since January. I am on my second round of Vancomycin. I really want to get the Covid vaccine soon. Can I or should I wait until this gos away?
I got my first Moderna shot February 5 and the second one on March 2. Before all that I stepped on glass with my big toe and was prescribed Cephalexin 500 2X and Clindamycin 4 times a day. My doctor thinks thats how I got C Diff. Taking Metronidazole 500mg 3 X for 10 days. I feel better now after a week.
My gastro physician suggested for me to list clindomycin &all myicins as problems for myself. I got CDiff after my second shoulder surgery. It was the drug that caused my c-diff .
I’ve just been diagnosed with CDiff …my gastro Doctor is prescribing Dificid to treat it. I have an appointment on 3/22 for the Covid vaccine. Is it safe to get it if I’m being treated for CDiff?
Kathie, definitely speak with your doctor but my understanding is that it shouldn’t matter.
I took my last vacomycin antibiotics 3/26/21. I think I just got over cdiff is it safe to take a covid shot ?
I wouldn’t. I’m in midst of C Diff infection right now. Taking Dificid. My doctors said do not get C19 vaccine during this time. Plus give body time after for GI to repopulate using probiotics
I have had cdiff for 6 months now. I had diverticulitis and asked if there was another drug other than flagel to take. Well the GI Dr put me on what I now know is in the top 3 drugs that give you cdiff. After complaining for two week of diarrhea I landed in the hospital. Took vancomycin for 14 days. The same Dr wanted me to taper off almost immediately. I waited to day 10. It did not go away. I went to a new Dr who put me on Difcid. I felt better after the 10 day course, but 3 days later it came back. I recently went on Difcid for 30 days. I tested negative for the toxins but unfortunately tested positive for GDH! That means cdiff has made a colony. I am back on Difcid. I received my first Covid vaccine on the 10th day off Difcid. Everything went well, but then tested positive for GDH a week later. I don’t think it had anything to do with the vaccine. I get my next vaccine next week. I am due to be off Difcid for 4 days when I get the vaccine. I hope all goes well. I am truly scared I will never get rid of this horrible cdiff. The cleaning is overwhelming. I started taking florastor hopefully it will help restore good gut health. Any suggestions as to what to do would be greatly appreciated.
Hi karease. I’m currently on vancomycin 250mg 4 x a day… antibiotics don’t just kill d bad bacteria but the normal flora or good bacteria in our gut too… that’swhy i think c diff is unending cycle to others. Decided to see a naturopathic doctor today who specializes in c. Diff colitis…. hope and pray that it would completely eliminate the c. Diff. You can do some research too re: naturopathic doctors or natural healing if you want….. just sharing.
Lots of probiotics (look for good brand with 10 strains)…add Sacromycees boularrdi too.
Fermented foods help…sauerkraut, etc.
Stay away from antacids
Hi, I realize it’s been awhile, but I’m curious how you did with the vaccine after finishing dificid? And how are you doing now?
I had my first Pfizer vaccine 3 weeks ago. I was due for my second today and had to cancel because I just tested positive for CDIF.
Hello,
Had you taken any antibiotics? Do you have a hx of C Diff?
I developed c diff the morning after my first Moderna shot 12/22. It has recurred twice now, I have been on vanco since Christmas. Shot did not cause the c diff; combo of clindamycin and moxifloxacin for diverticulitis did it. Got second shot at 5 weeks, as c diff recurred, and I wanted an extra week of vanco on board before getting it.
I am a health care provider, I am so sick I am leaving my practice next week. End of a 25 year career. Doing the legwork to establish protocol for FMT at our rural hospital.
I got my moderna vaccine and then got cdiff it is correlated when I told people that they laughed this thred is confirming my thoughts. I have not been on antibiotics in years-and have been pretty much isolated for two. I am on my third case of cdiff and i feel like I am dying anyone have any suggestions other than fecal transplant and suing moderna that’s what I get for taking a drug I didn’t know what was in it
I have had c-diff for almost a year now, after taking clindamycin. I battle with diarrhea everyday. I vave been on Flagyl, Dificid, and currently on Vancomycin 1000 mg a day. I am waiting for a Fecal Transplant. Which due to covid they have halted until further notice. I have been hospitalized 2 times in the past year for it. I was septic the first time and was very ill. I struggle daily with food, everything I eat goes right through me. So I try not to eat. I am constantly exhausted, in pain and on the toilet. I received my first Moderna Covid shot 6 days ago. My stomach is in constant turmoil since then, it has become worse. I have only been able to eat crackers and toast, and still my symptoms are horrible. Constant cramping, gas, pain and diarrhea. This disease is no joke. You cannot possibly have a normal life, while you are battling it. Although God knows I try. I work full time as a nurse, and have 5 beautiful grandchildren, that I see as much as I can. But my symptoms keep me from doing alot of the things I want to do. I have hope that I am going to have my transplant, in the upcoming months. Until then, I take everyday as it comes. With a smile, or is that a grimace on my face. Oops gotta run!
I have had CDiff 2x. My last bout was last July and I ended up in the ER. Lost 11 pounds in a week. Ended up on vacomycin and that did help me. I had a UTI and was given one antibiotic and two days later, was given another because she said it was a different type of infection and needed this med. This is how I got CDiff. The first medication the doctor put me on or CDiff did not help. Actually, made it worse. Finally got the V and it helped. My concern is taking the vaccine. Will this cause any issues??
Gwen there is no normal life with cdiff. I am 53 had not been on antibiotics in years. Got my moderna vaccine then got cdiff. I have had three recurrences since September and the cleaning is overwhelming and it is awful I never knew it existed. Blessings to you Laura
I’ve had cdiff for over 7 year’s and multiple fecal transplant FMT after my first shot positive again
My 82 year old mom has dealt with Cdiff for over a year. We do not know where or how she even got it. She has been treated with V very successful, as long as she stays on it. She recently received an Immune IV therapy, which was supposed to have a great success rate! She was doing fine UNTIL she received her Covid vaccine….she has now relapsed again. I have to wonder the connection between the vaccine and a “sudden” return of Cdiff? Now her option is to treat with V, and then stay on one pill every day for the rest of her life. I can find nothing that connects my opinion, but wonder how many relapse after getting one of these vaccines? It might be years before it is tracked or really reported. Anyone have a similar story?
I’m a 76 yr old who had appendix surgery in April and given lots of IV anitibiotics. Diarrhea started a week out of the hospital. Not knowing anything about Cdiff, I waited 2 more weeks to see my doctor. She didn’t tell me anything to do other than take Vancomycin and use a separate bathroom. Thank goodness for the internet! After my 2nd Rx of Vancomycin (tapered the 2nd time), taking Florastor, Allicin, and Sulforaphane Glucosinolate , I am happy to say I’m feeling good after my last antibiotic a week ago. Keep your fingers crossed for me… If I have a setback, I’m going to an integrative physician!
I also got c dif 5 days after the first covid shot, and had it for 4 months. Vanco just kept the situation under control, but it was dificid that finally knocked it down. I take Align and Florastor for maintenance. My gastro doc told me no more Mrna shots for me. So I am in total defense mode and practicing all guidelines, for the rest of my life. Hopefully something better will come along for us immuno compromised due to Immuran for Chrohn’s.
Lynn I got the moderna vaccine and then got cdiff I was not on antibiotics in over three years. I am on my third round of cdiff and it is a gamechanger.
I started having problems with weakness, weight loss, nausea shortly after having my gallbladder removed. I was told this is normal so I didn’t see a Dr. On Feb 2nd I had my vaccines then all symptoms git worse. Currently on mitro it’s theb6thbday and isn’t getting any better.
I completely sympathize with all of you. I was diagnosed with cdiff in March after some dental work. Since then, I’ve been on Vancomycin, Flagy, and another round of vancomycin tapered. Just recently I was found negative for Cdiff and am extremely thankful to God. I know because of him I’ve been able to overcome it. I do have some questions. Since being on the meds I’ve noticed some extreme anxiety and nerve issues. I often feel like I have goosebumps and feel out of breath. My mouth and chest feel cold on occasion as if I just ate a mint. It’s a very weird sensation. I’m working with a nutritionist to help with digestion and weight loss too. Along with that, I d like to get the COVID vaccine but am terrified. Has anyone had these symptoms after antibiotics?
Rachel I get the chills and mouth and chest feel cold on occasion also. I got the moderna vaccine then got cdiff. I am having my third battle with a recurrence now. Antibiotics are not working. I pray to God for healing.
I had oral surgery and was given a round of 1000 mg Amoxicillin / 500mg 2x day precautionary to prevent infection end of Aug 21, Sept 21 I was diagnosed with Strep and let them know I took the Amox in Aug and was given Augmentin, felt better and ready to go to work a week to the day after diagnosis and work up with a fever which spiked to 104 and severe diarrhea like I had never had before. Saw a Doc 9/28 and had labs done, WBC 11k and after a mistake at the lab (label swap on sample containers and incorrect storage instructions for fecal tests) the samples most representative of what my body was putting out were deemed useless and I had to bring back new samples, which in my opinion were (sorry for being gross – undigested food), but they said I did not have C-Diff. I kept running low grade fevers and was exhausted, refused care with appt at PCP and went back to another location seeing sick patients, need labs (blood, additional stool, and CT Scan ordered). I made appointments but the abdominal pain was so severe I could not take it anymore (also recurring with my 15 or more trips to the bathroom daily). I wrote to the treating Dr. and they called and told me to go to the Emergency Room instead of waiting to go to the outpatient appointments, since it was so late and I did not think I would get a CT that night, I could not drive myself and the ambulance would have taken me to a different hospital I went to bed and planned on going first thing in the am. Woke up with 104 again, same as the beginning of month long nightmare, took some Tylenol and went back to bed or a few hours and went to the ER since I knew I would be staying there and needed to get showered and grab a few things (no hate please – I just know the drill). They took my vitals and took blood and began an IV in the waiting room of the ER I was that bad. I was dehydrated, my blood pressure was 71/44, I lost 20 lbs, my WBC was at or over 40k and after the CT Scan and test of a sample, I was confirmed to have C-Diff. I did have both Covid Shots in April so I do not think my covid vaccinations had anything to do with the C-Diff. I also had taken both antibiotics and far stronger ones in the past with no issues. Thankfully Vanco worked for me and I was released in two days with a normal WBC. I was released on the 17th Oct and was told to get a Flu and my Booster Covid shot on the 16th of Nov and wondering if anyone else has done this recently after a severe infection. My bowel movements are back to normal, I am still watching my diet since I am afraid to upset my gut with anything difficult to digest. I see a ton of Probiotics on the market with different claims and strains and no clue which one to pick up. Lactobacillus is what I was told to look for, anyone have success with any particular pro-biotic? Thanks
I started loosing weight quickly about 3 months ago. Around August 25, 2021 I noticed I lost 10 pound without trying. Despite trying to overeat, I’m down 45 pounds as of Nov 29th. I just found out I have C-diff. This is the first time I have ever had this. I hadn’t had any antibiotics or anything. The only thing I can think of is I had gotten my COVID vaccines right around then. My first shot was July 28th and my second was August 20. Is it possible?
Cassandra yes I found the same correlation. Moderna vaccine then cdiff. Just awful. I am on my third recurrence. It is awful. I a53 and never knew it existed.
I had C-diff. infection at the end of July. I had very high fever, diarrhea, totally exausted, ended in hospital. The diagnose was C-diff. I took Metronidazol. I took klindamycin two weeks before it happened. At that time my little baby was only two months. I am from Europe and many doctors does not have knowledge about this infection. Metronidazol did work me although I had bad headaches and depresion. I take probiotics and Saccharomyces boulardii. In USA it is Florastor. In the middle if august diarrhea started again. I was tested, no toxins but GDH positive. They gave mi Metronidazol again. I am ok now, stool is formed but 3 times a day, I eat more so maybe it’s the reason for more often bowel movement. I was very underweight. Could someone tell me what exactly do you eat? The doctors told me no dairy products, no fresh vegetables, no nuts, only apple puree, green banana, cocked carrot, celery, rice, potatos, lean chicken meat, white bread. No fiber.
I am startig to worry about the nutritions. Can normal food cause C-diff. back?
Because I worry so much that it will come back. I thought I was going to die. In here vanco or difficid can give you only in hospital intravenous and I do not want to leave my baby again. I was heart broken.
I never really got a good diet plan either when I had it, I still suffer from stomach pains, I use the Saccharomyces boulardii probiotic as well, mainly when I feel symptoms start to return or just in general get diarrhea. At the time I was eating bagels with peanut butter, or eating white rice, a banana at times. But of course can’t live off that for too long. For a short period of time, that was all I would take in. Oh, and I did have Greek yogurt as well. Vancomycin was what I was taking during the time. I had to go through 4 rounds of that. I never had to get that done in the hospital or anything, it was an antibiotic given.
Two words: Fecal Transplant only “cure” for C Diff. I have Covid and hope I don’t get C Diff, don’t plan on getting the vaccine, but wish the stupid Veterans Affairs had got me the fecal transplant. I now have horrid IBS and low quality of life from multiple Vancomycin runs to include 2 long tapers. Ask for fecal transplants and deny antibiotics esp C Diff round 2 and beyond. I have had it once due to antibiotics and then because of Proton Pump Inhibitors (Omemprezole and other heartburn meds).
From all the comments, it appears there may be a connection to getting C-Diff after having Covid. I had Covid and got over it fine. Then a few days later, I had my second case of C-Diff. I had no antibiotics before or after the second case of Covid.
I picked this blog due to people feeling there is a link between Covid and Cdiff. Based on what I’m reading here and my own experience, it appears the antibodies somehow predispose one’s gut to getting Cdiff.
My partner got Covid when Omicron was starting to surge here. I got preventative monoclonal antibodies and none of my many tests ever were positive despite the monoclonal antibodies likely being ineffective against omicron. However, shortly after getting the antibodies, I developed the telltale signs of C-diff….20+ times explosive watery diarrhea a day, painful gurgly gut, horrible sickly sweet smell and losing bowel control even when sleeping. I lost about 8 lbs quickly because it either hurt to eat or just went right through me. Even the BRAT diet. This went on for some time. I knew I was taking a risk by not seeking medical treatment, and I came very close to doing so, but in our remote rural area it seemed medical care or hospitalization during a covid surge is also a risk. The limited providers here do not seem very informed and either give the wrong care (with bad outcomes sometimes) or refer out to specialists in big cities far away.
So I decided to lean on my medical knowledge, apply my research skills and then self-treat with supplements based on everything I’d learned. It cost me a lot of $$ but after 2 weeks of doing that, I went from feeling weak, dehydrated, malnourished and feeling like my GI system may never be able to function normally again, to regular food and GI function!
I feel I shouldn’t name everything I took and possibly influence someone to not take an antibiotic that may save their life, but I will share some things I took along with my treatment regimen that you can take along with antibiotics also. Such as, Manuka honey, which is believed to dissolve the protective biofilm on the Cdiff spores to help medication penetrate it and also prevent it from hiding out and reinfecting again. Also Florastor. Good stuff!
Soluable fiber like banana flakes, oat bran hot cereal that help slow/stop diarrhea and also clean out the Cdiff (eat it a couple hours or more apart from medications).
Hope this helps.
I’m 37 I had COVID the beginning of February. When I was on the tail end of it I started getting GI symptoms. I suffer from acid reflux and IBS. I started getting stomach cramps, loss of appetite, diarrhea in the mornings and sometimes other times of the day. I went to my primary doctor and they did a CT scan and said my insides looked great. Gave me more antacids and antispasmodic and sent me on my way. I kept having symptoms. A bit less every week but still had no appetite and a lot of discomfort when I ate. I went to the gastro and they ordered a stool sample. They say I have C.Diff and that they are putting me on antibiotics. The weird thing is that my test said detect C.diff toxin (A,B), PCR but negative for colonization and no c diff infection. They didn’t explain anything. I haven’t gotten the antibiotics yet and I feel better. The diarrhea is gone. I still feel somewhat bloated and I’m getting my appetite back but I’m still eating a bland diet and I’ve been taking probiotics for a while.
Could I have been misdiagnosed?
I took the first and second shot of Moderna and had no GI symptoms I do not have the booster shot yet and I’m afraid.
Reading up on C.diff it seams like very scary disease. I already have Graves that took 3 months to diagnose and was bad and Psoriasis which I take immune suppressants for. Had my gallbladder removed. I’m terrified of having another thing to have to fight through.
I’ve had bad experiences with doctors and have been misdiagnosed before and given a pill that gave me the most horrific allergic reaction. I have massive Anxiety when it comes to Illness.
Good luck to everyone suffering from this. I wish us all the best.
Hi it is awful to have cdiff and just having had a baby. I have had three recurrences of cdiff. It makes you feel like you are going to die. I am on a medical food liquid diet called elemental diet that is prescribed by my doctor. It helped get rid of the second round but it came back when I went off the elemental liquid diet. The two rounds of antibiotics I received to treat cdiff did not work. The elemental diet and a probiotic called kiefer worked. It is awful I worry about the nutrition but the elemental liquid diet give a lot of nutrition.
Dear Laura, I am so sorry to hear you still fight cdiff. I was partly on elemental liquid diet, it helped. I am 8 months after second relapse and I am ok for now. I still do not eat dairy products or fresh vegetables, no nuts, no legumes. Did your doctor told you about Dificid (fidaxomicin)? It is used when metronidazol and vanco fails. It heleped many people. FMT is the last (and only) option, when everything else fails.
I hope you will get better soon. All the best to you.
Can you get recurring cdiff from using antiseptic mouth
1 month after the vaccine I had c diff. The pain I am in is comparable to child birth.
There has been correlation but no causation found to the vaccine. It will remain like this until a memo is leaked from Moderna.
I was fine before the vaccine now my gut is now destroyed. I lost 30 lbs in 2 weeks. I can eat 8 foods now. Had every test possible there is nothing they can find.
I am screwed