It’s World Hand Hygiene Day: Are Your Caregiver’s Hands Clean?
Other Categories
Written by Trish Pooley
It was 1846 when Ignaz Semmelweis, a Hungarian doctor at Vienna General Hospital, discovered how hand washing could save lives. Social medicine considers him to be one of the early “physician scientists.” Practicing in hospital maternity wards, he became intent upon understanding why so many women died of “childbed fever” after giving birth.
He began to create hypotheses for which he gathered data. He observed that the women whose care was provided in the ward by male doctors or medical students resulted in five times the mortality rate. Those women whose care was provided in the midwives’ clinic did not die of childbed fever nearly as often.
After testing several different theories, he found himself frustrated until a pathologist colleague in the hospital died of the fever and its complications. Realizing that each woman who died of childbed fever had been autopsied, he focused his attention on this practice. The dead pathologist had pricked his finger while performing an autopsy on a patient who had died of this diagnosis. This led Ignaz to make the association between hand washing and reduced infection rates, a critically important tool. (1)
This was 1846. It is now 2017. Despite knowing that hand washing can prevent many infections, policy and/or practice continue to lag well behind science. This is the same point made in a recent TIME magazine article on preventing pandemics. “Even as the scientific and international communities have begun to take the threat of pandemics more seriously, global health experts—including Bill Gates, World Health Organization Director Dr. Margaret Chan and former CDC Director Dr. Tom Frieden, to name just a few—warn that nowhere near enough is being done to prepare, leaving the U.S. scarily exposed. That’s because the system for responding to infectious disease is broken.” The Ebola epidemic demonstrated how SLOW our response can be. (2)
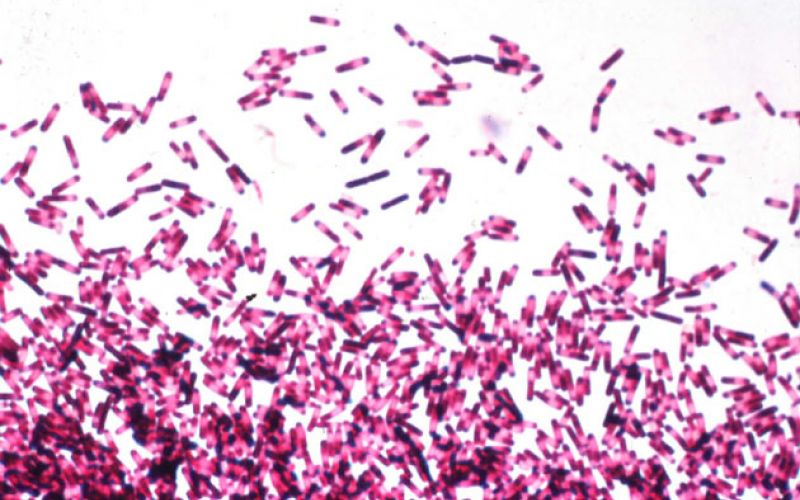
Our response in this country to reducing infections from Clostridium difficile is equally slow. This is one of the most common known environmental pathogens in hospitals and clinics, but while we were screening patients for travel to West Africa to prevent the spread of Ebola to this country, we were not doing any regular education about C. diff or screening. And most hospitals rely on alcohol based gel dispensers for handwashing when science has demonstrated that only soap and water or bleach will kill C. diff on hands, high touch surfaces, and curtains or scrubs. So, C. diff continues to kill approximately 29,000 people each year.
Like the CDC, Dr. Semmelweiss created a protocol for handwashing with soap and water or chlorine which his colleagues followed reluctantly while noting that childbed fever infections fell and fewer women died. But, they disliked Dr. Semmelweiss’s churlish insistence on this practice, feeling that they were somehow being indicted for transmitting this infection to their patients. They claimed that handwashing just “took too much time,” a complaint we still hear today. It was a challenge to gain compliance even if their own health and life could also be protected. Ultimately, Dr. Semmelweiss lost his job.
The challenge of gaining handwashing compliance in 2017 remains. A recent article in Becker’s Hospital Review for Infection & Clinical Quality listed ten findings on improving hand hygiene (summarized):
- Peer pressure: All hospital employees got paid a $1200 bonus if the hospital met its overall target.
- Background music was played while the necessary handwashing times were met.
- Text-messaging of congratulations or encouragement if handwashing compliance was met during surveillance.
- Physicians were instructed to offer patients the proper hand sanitation, thus prompting them to model this themselves.
- Building a positive culture being paired with automated handwashing surveillance systems.
- Bedside handwashing improved with extra healthcare workers in the room to prompt or cue one another.
- Using a multifaceted educational intervention on a hospital-wide basis.
- Auditing and providing feedback.
- Measuring compliance when entering and leaving a patient room.
- Implementing a “safety stand down” to stop nonessential hospital activities on units to discuss action plans to improve hand hygiene.
It has been suggested that patients must become the new superheroes of medicine by taking responsibility for ensuring good antibiotic stewardship. If doctors do not see the need to take ownership of good antibiotic stewardship practices, then perhaps patients must initiate responsibility for proper hand hygiene compliance as well. The tips listed above provide ideas in doing this. Here are a few I have used:
- Doctors are not our peers, but they are our partners. Model the behavior we want. Wash your hands in the presence of the doctor entering your room. Invite the doctor to do so while smiling and moving out of the way.
- Use a music based intervention with your iPhone to play music for the 21-30 seconds required for optimal hand washing or sing for 21 seconds (try the “Happy Birthday” song or “Yankee Doodle”).
- Text message them your appreciation using an emoji understood to be encouragement, or plant a little sticker on their white coat letting colleagues know they practice handwashing. When we vote we get a sticker saying “I voted.” Make stickers with the meme “I wash because I care.” Create your own.
- Invite the physician to offer a hand sanitizer or a reminder to use soap and water for others in the room. Let it be their idea to model this behavior.
- Reinforce the healthcare worker on your team who is most rigorous with hand hygiene compliance by filling out a feedback card noting this (be creative). Offer to bring this person a coffee or snack to enjoy when they take their break. I’ve done this and watched handwashing compliance skyrocket.
- Use the military stand down technique by insisting that all other activities stop until hand hygiene has been completed. Then, and only then, proceed to the medical history review, medication delivery or IV changes. It’s really this important.
- Use signs, badges, or bookmarks bearing the message “I wash because I care” or “save that line” with reminders that handwashing is one of the most important healthcare tools we have had since 1846. Thank everyone who plays along with you!
No one listened to Dr. Semmelweis for years. He wrote a book about all he had learned but died in a mental institution in 1865. It was Louis Pasteur who further validated his theories.
If you have had C. diff or still do, you know how important scrupulous hand hygiene is. Do not be afraid to let the healthcare professionals on your team know why this is important to you. They will leave their egos at the door in response because they care. Handwashing saves lives.



Leave a Reply